by Lara Spector ND
Over 50% of women will suffer from a urinary tract infection (UTI) during their lifetime. One-third to one-half of these women will have a recurrent UTI within one year. Recurrent UTIs are defined as three or more UTIs in a 12-month period.[1] The most commonly used conventional therapies for these conditions are antibiotics. There is increased awareness and concern about antibiotic resistance with repetitive use of these medicines. This growing concern has created an interest in alternative treatments for UTIs. The purpose of this article is to discuss this condition as well as the causes and alternative treatments for cure and further prevention.
This article will also illuminate the link between UTIs and an imbalanced gut microbiome, otherwise known as dysbiosis. Gastrointestinal conditions associated with dysbiosis such as irritable bowel syndrome (IBS) and small intestine bacterial overgrowth (SIBO) are common in those with bladder infections.
Urinary Tract Infections (UTIs)
Definition and Symptoms
UTIs are the most common bladder infection and are associated with symptoms such as burning with urination, increased urinary frequency and urgency (in the absence of vaginal discharge), and significant pain. Diagnosis can be made on symptoms alone, though most doctors will require a urinalysis to identify the presence of infection to prescribe antibiotics.
Cause
 |
E. coli from the gastrointestinal system is the cause of 80–85% of urinary tract infections. Sexual activity is researched to be the cause of between 75 and 90% of these infections in premenopausal females, with more frequent intercourse increasing the risk of infection.[2] UTIs in the postmenopausal female are not related to sexual activity; instead, they are related to the decrease in estrogen levels and resulting vaginal atrophy and loss of beneficial vaginal flora in this population. Other risk factors include genetics and diabetes.[3] |
Treatments
Conventional Treatment: Antibiotics
Conventional treatment of UTIs rely on antibiotics, which are estimated to cure 80–90% of uncomplicated UTIs. The most common antibiotics include nitrofurantoin (commonly known as Macrobid) and trimethoprim sulfamethoxazole (TMP/SMX). Growing concern surrounds the repetitive use of these antibiotics as resistance has been shown to occur, as well as an increase frequency of candidiasis following use.[4]
Naturopathic Approach
Prevention
As mentioned above, the largest causative factor for UTIs is sexual activity. It is recommended to urinate and allow for complete bladder emptying postintercourse as a preventative technique for UTIs. Drinking enough water is also a known preventative strategy for UTIs. A study looking at 140 premenopausal women who suffered from recurrent UTIs noticed they were drinking a lot less than the recommended amount of water daily, which is 64 ounces of water a day.[5]
Probiotics
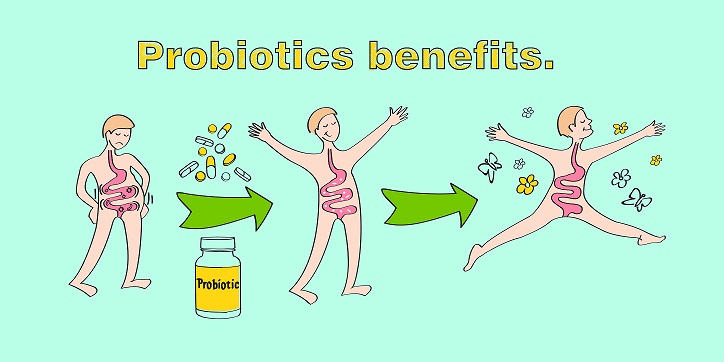 |
As most UTIs are the result of E. coli from the digestive tract, promoting healthy microflora ratios is beneficial in preventing and treating UTIs. Three Lactobacillus strains—L. acidophilus, L. rhamnosus, and L. reuteri—have been studied to prevent UTIs and also showed no increase in antibiotic resistance.[6] |
Cranberry
|
This herb has been shown to inhibit the binding of E. coli to the epithelial cells lining the bladder wall. A Cochrane review and meta-analysis revealed that cranberry significantly reduced the chance of developing a UTI. It has also been shown to significantly reduce the biofilm load. This herb has been found to be effective in the form of pure juice, capsules, and tableted extracts.[7] |
 |
Uva ursi
 |
This herb, along with cranberry, is one of the most commonly used antibacterial agents for UTIs. It is best used when the urine pH is more alkaline, above 8, as the main antimicrobial constituent in this herb, arbutin, is released in alkaline urine.[7] |
D-Mannose
This is a simple sugar that, like cranberry, prevents adhesion of E. coli to the epithelial cells lining the bladder.[7] In a 2014 study that compared D-mannose to nitrofurantoin, D-mannose significantly reduced the risk of recurrent UTIs and showed a significantly lower risk of side effects.[8]
The Link to Common Gastrointestinal Conditions such as IBS and SIBO
To read more about IBS and SIBO, please see my original article at https://www.naturopathiccurrents.com/articles/sibo-small-intestinal-bacterial-overgrowth. The underlying root cause for both IBS and SIBO is dysbiosis, or an imbalanced microflora in the gastrointestinal tract. There has been an increased correlation with these gastrointestinal conditions and UTIs.[9] An article by Ojetti et al has identified that the treatment of constipation from SIBO may avoid the reinfection of E. coli in the urinary tract from the rectal reservoir.[10] The treatment of IBS and/or SIBO is mentioned in my article referenced above.
Conclusion: A Well-Rounded Approach to UTIs
Numerous studies demonstrate the effectiveness of natural substances for prevention and treatment of UTIs. The most studied of these are discussed in this article, including cranberry, Uva ursi, D- mannose, and probiotics. The increased prevalence of UTIs occurring concurrently with conditions such as IBS and SIBO suggests the need to address these gastrointestinal ailments in conjunction with using the above-mentioned therapies for UTIs. A well-rounded approach for UTIs which addresses dysbiosis in the gastrointestinal tract, as well as using the above natural UTI remedies, shows promise for treatment and long-term prevention of UTIs.
References:



